Type Four Rta
The Evolution of Type Four RTA: A Comprehensive Analysis
Introduction
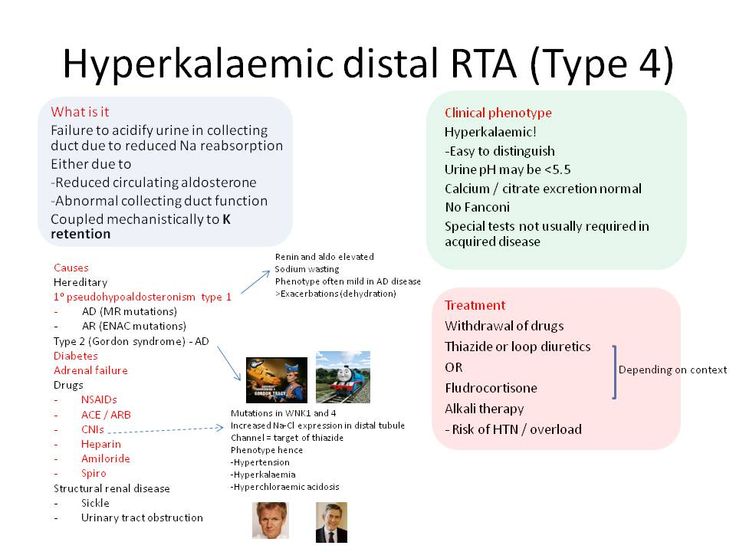
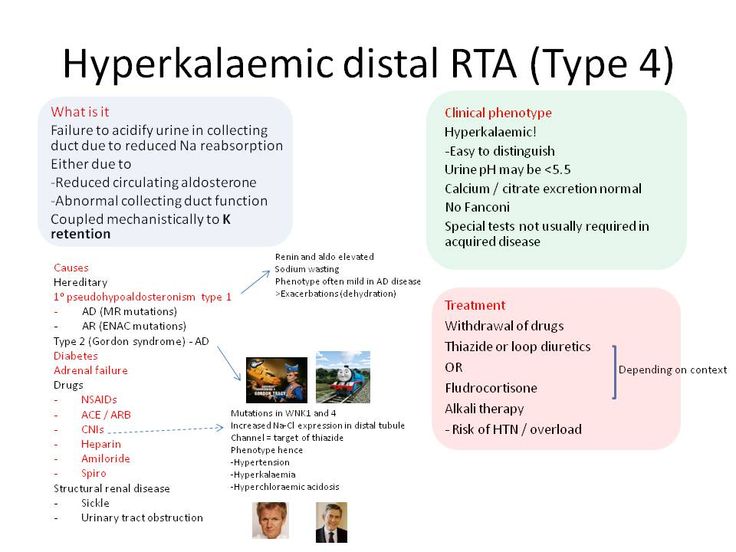
Renal Tubular Acidosis (RTA) is a heterogeneous group of disorders characterized by impaired renal acidification, leading to metabolic acidosis. Among its subtypes, Type Four RTA (T4RTA), also known as hyperkalemic RTA, stands out due to its unique pathophysiology, clinical presentation, and management challenges. Unlike other forms of RTA, T4RTA is often associated with hypertension, hyperkalemia, and aldosterone resistance. This article delves into the historical evolution, pathophysiological mechanisms, diagnostic criteria, treatment modalities, and future trends of T4RTA, providing a holistic understanding of this complex condition.
Historical Evolution of RTA Classification
The classification of RTA has undergone significant revisions since its initial description in the early 20th century. The distal RTA (Type 1) was first identified in 1935, followed by the recognition of proximal RTA (Type 2) in the 1960s. Type Three RTA (T3RTA), a mixed form, was later described. However, it was not until the 1970s that Type Four RTA was distinctly classified, primarily due to its association with aldosterone resistance and hyperkalemia.
Key Milestones in RTA Classification
- 1935: First description of distal RTA.
- 1960s: Identification of proximal RTA.
- 1970s: Recognition of Type Four RTA as a distinct entity.
Pathophysiology of Type Four RTA
T4RTA is characterized by aldosterone resistance in the distal nephron, leading to impaired potassium secretion and hydrogen ion (H+) excretion. This results in hyperkalemia and metabolic acidosis. Unlike other forms of RTA, T4RTA is often associated with hypertension due to volume expansion and impaired sodium excretion.
Key Pathophysiological Features of T4RTA:
- Aldosterone resistance in the distal nephron.
- Impaired potassium and hydrogen ion secretion.
- Hyperkalemia and metabolic acidosis.
- Hypertension due to volume overload.
Aldosterone Resistance vs. Aldosterone Deficiency
Aldosterone Resistance (T4RTA): Normal or elevated aldosterone levels with impaired renal response.
Aldosterone Deficiency (Addison’s Disease): Low aldosterone levels due to adrenal insufficiency.
Clinical Presentation and Diagnosis
Patients with T4RTA typically present with nonspecific symptoms, including fatigue, muscle weakness, and polyuria. Laboratory findings are critical for diagnosis and include:
- Hyperkalemia (serum potassium > 5.5 mEq/L).
- Metabolic acidosis (serum bicarbonate < 22 mEq/L).
- Normal anion gap.
- Hypertension in most cases.
Diagnostic Approach for T4RTA
- Step 1: Measure serum electrolytes (potassium, bicarbonate) and pH.
- Step 2: Assess urinary pH (typically > 5.5 in metabolic acidosis).
- Step 3: Evaluate aldosterone levels and renal response to fludrocortisone.
- Step 4: Exclude other causes of hyperkalemia (e.g., chronic kidney disease, medications).
Treatment Modalities for T4RTA
Management of T4RTA focuses on correcting hyperkalemia, metabolic acidosis, and hypertension. Treatment options include:
First-Line Therapies
- Bicarbonate Supplementation: To correct metabolic acidosis.
- Potassium-Binding Resins: To reduce hyperkalemia.
- Thiazide Diuretics: To enhance potassium excretion and manage hypertension.
Challenges in T4RTA Management
Pros: Effective correction of acidosis and hyperkalemia with available therapies.
Cons: Risk of volume depletion and electrolyte imbalances with diuretics.
Comparative Analysis: T4RTA vs. Other RTAs
Understanding the distinctions between T4RTA and other subtypes is crucial for accurate diagnosis and management.
| Feature | Type Four RTA | Type One RTA | Type Two RTA |
|---|---|---|---|
| Hyperkalemia | Yes | No | No |
| Hypertension | Common | Rare | Rare |
| Aldosterone Status | Resistant | Normal | Normal |
Future Trends and Emerging Therapies
Research into T4RTA is advancing, with a focus on genetic predispositions and novel therapeutic targets. Emerging therapies include:
- Aldosterone Receptor Modulators: To improve renal response to aldosterone.
- Gene Therapies: Targeting mutations associated with aldosterone resistance.
Potential Breakthroughs
- Personalized medicine based on genetic profiling.
- Development of non-invasive diagnostic tools.
FAQ Section
What causes aldosterone resistance in Type Four RTA?
+Aldosterone resistance in T4RTA is often due to genetic mutations or acquired conditions affecting the distal nephron’s ability to respond to aldosterone.
Can Type Four RTA be cured?
+While there is no cure, T4RTA can be effectively managed with medications and lifestyle modifications to control symptoms and prevent complications.
How is T4RTA different from Type One RTA?
+T4RTA is associated with hyperkalemia and hypertension, whereas Type One RTA presents with hypokalemia and normal blood pressure.
Conclusion
Type Four RTA is a complex disorder requiring a multidisciplinary approach for accurate diagnosis and management. With advancements in genetic research and therapeutic interventions, the future holds promise for improved outcomes in patients with this condition. Understanding its unique pathophysiology and clinical presentation is essential for clinicians to provide effective care.